
Diabetes, or diabetes mellitus (DM), is a metabolic disorder in which the body cannot properly store and use sugar.
It affects the body's ability to use glucose, a type of sugar found in the blood, as fuel. This happens because the body does not produce enough insulin, or the cells do not correctly respond to insulin to use glucose as energy.
Insulin is a type of hormone produced by the pancreas to regulate how blood sugar becomes energy. An imbalance of insulin or resistance to insulin causes diabetes.
Diabetes is linked to a higher risk of cardiovascular disease, kidney disease, vision loss, neurological conditions, and damage to blood vessels and organs.
There is type 1, type 2, and gestational diabetes. They have different causes and risk factors, and different lines of treatment.
This article will compare the similarities and differences of types 1 and 2 diabetes.
Gestational diabetes occurs in pregnancy and typically resolves after childbirth.
However, having gestational diabetes also increases the risk of developing type 2 diabetes after pregnancy, so patients are often screened for type 2 diabetes at a later date.
According to the Centers for Disease Control and Prevention (CDC), 29.1 million people in the United States (U.S.) have diabetes.

In type 1 diabetes, the immune system mistakenly attacks the insulin-producing pancreatic beta cells.
These cells are destroyed, reducing the body's ability to produce sufficient insulin and regulate blood glucose levels.
The body does not produce insulin, so the person needs supplemental insulin from the time they are diagnosed.
It often affects children and young adults, and it can start suddenly.
When type 2 diabetes starts, cells become resistant to the effects of insulin. In time, the body stops producing enough insulin, and the body can no longer use glucose effectively.
This means the cells cannot take up glucose, and glucose builds up in the blood.
This is called insulin resistance. If blood glucose is always high, the cells will be overexposed to insulin. They become less responsive or unresponsive to insulin.
Symptoms may take years to appear, and people can often use medications, diet, and exercise from in the early stages to reduce the risk or slow the disease.
People in the early stage of type 2 diabetes do not need supplemental insulin, but as the disease progresses, this may be necessary to control blood glucose control and to survive.
Type 2 often results from obesity and lifestyle and dietary factors, as well as medications and other issues.
Diet has been linked to type 2 diabetes, but early diet may also have an impact on type 1.
Type 1 has sometimes been found to be more common in those who were introduced to cow's milk at an earlier stage. This suggests that breast-feeding for longer may reduce the risk. However, more research is needed.
Type 2 tends to be common in families where obesity is also a family trait. There may be a genetic link, or this may be because families have similar eating and exercise habits.
Diets high in simple sugars and low in fiber and vital nutrients have been linked to diabetes.
The consequences of persistently high levels of blood glucose can differ between types 1 and 2, but some symptoms and warning signs are common to both types.
The most serious complications involve kidney failure, eye problems and vision loss, neurological damage and increased risk of cardiovascular problems, including heart attack and stroke.
The table below shows some signs and symptoms of possible complications.

Common physical attributes: BMI is mostly within the normal range or low.
Onset: Rapid, often presenting acutely with ketoacidosis
Warning signs:Extreme thirst and hunger - Frequent urination - Rapid weight loss - Extreme weakness and fatigue - Nausea, vomiting - Irritability
Complications: Diabetic coma or ketoacidosis - High blood pressure - Hypoglycemia, or low blood sugar - Nephropathy, or kidney disease - Blindness - Heart attack - Stroke - Neuropathy - Amputation - Ulcers
Common physical attributes: BMI is in the overweight or obese range.
Onset: Slow, sometimes taking years and often presenting without early symptoms
Warning signs: Extreme thirst and hunger - Frequent urination - Rapid weight loss - Extreme weakness and fatigue - Nausea, vomiting - Irritability - Blurred vision - Skin infections - Sores that heal slowly - Dry, itchy skin - Pins and needles or numbness in feet
Complications: Diabetic coma or ketoacidosis, due to high blood sugar - High blood pressure - Hypoglycemia, or low blood sugar - Nephropathy - Blindness - Heart attack - Stroke - Neuropathy - Amputation - Ulcers

The onset of type 1 diabetes tends to be sudden. If symptoms are present, the person should see a doctor as soon as possible.
A person with prediabetes and the early stages of type 2 will have no symptoms.
If a routine blood test shows that blood sugar levels are high, action can be taken to delay or prevent diabetes and its complications.
Any of the following tests can be used for diagnosis of type 1 or type 2 diabetes, but they are not all recommended for diagnosing both types:
Another blood test, the random plasma glucose (RPG) test, is sometimes used to diagnose diabetes during a regular health check.
 What Happens When You Quit Smoking – A Timeline
What Happens When You Quit Smoking – A TimelineEvery year more than 7 million people die as a result o...
 Types Of Yoga, Which One Is Best For You?
Types Of Yoga, Which One Is Best For You?There are two types of people in the world - those who ...
 10 Amazing Health Benefits Of Apricot Juice
10 Amazing Health Benefits Of Apricot JuiceOriginally from China, the use of apricots began almost...
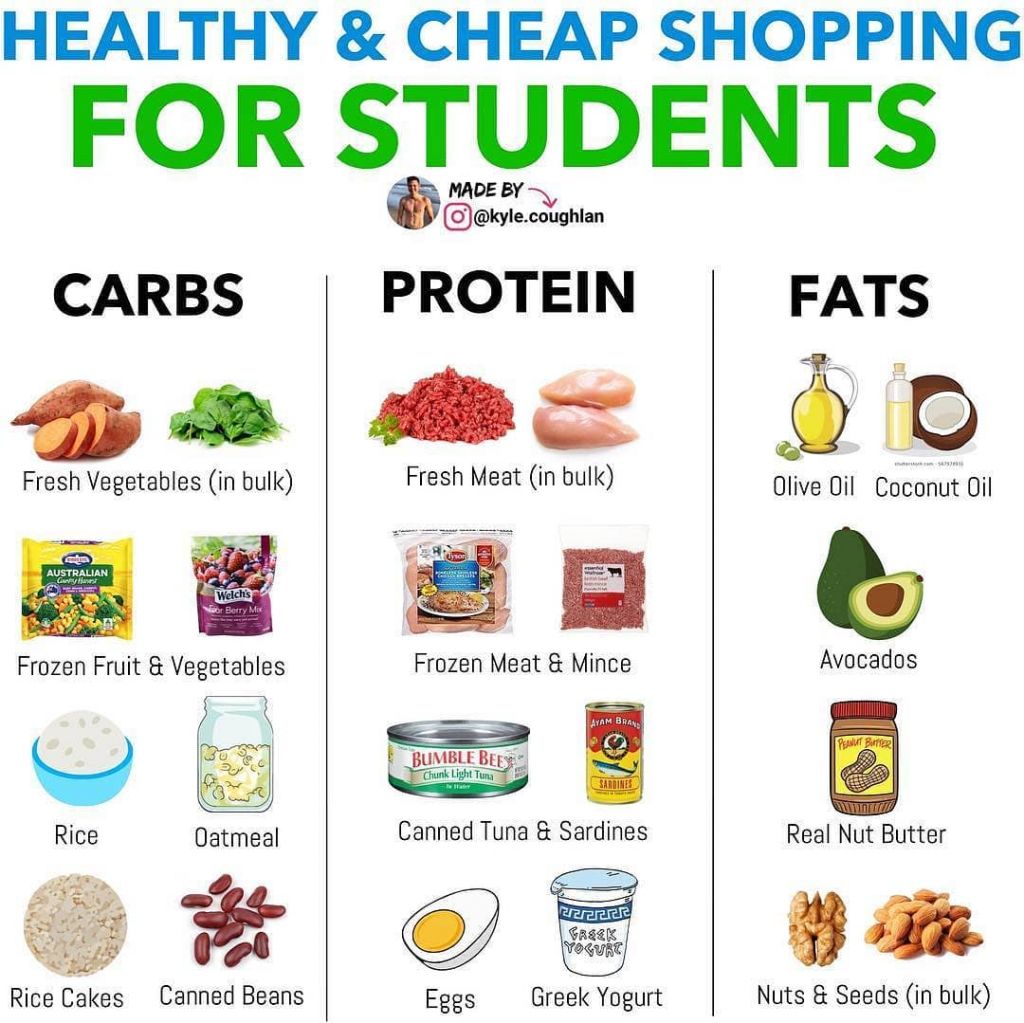 Cheap & Healthy Shopping List for Students
Cheap & Healthy Shopping List for StudentsCheap & Healthy Shopping List for StudentsStaying o...
 This Honey, Lemon And Cinnamon Drink Will Help You Lose Pounds In A Week
This Honey, Lemon And Cinnamon Drink Will Help You Lose Pounds In A WeekThe most effective way to lose weight is to do aerobic ...
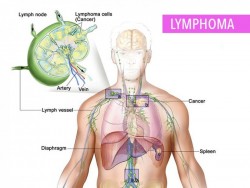 What You Need To Know About Lymphoma
What You Need To Know About LymphomaLymphoma is a cancer of the lymphatic system. It affect...
 This Honey, Lemon And Cinnamon Drink Will Help You Lose Pounds In A Week
This Honey, Lemon And Cinnamon Drink Will Help You Lose Pounds In A WeekThe most effective way to lose weight is to do aerobic ...
 Colon Cancer: Could Exercise Halt Tumor Growth?
Colon Cancer: Could Exercise Halt Tumor Growth?New research published in the Journal of Physiology sug...